In 2010, I was fresh out of two consecutive births. With a newborn and an older child only 16 months older, I was 95% sure I was totally finished with having children.
That remaining 5%, however, kept me from getting surgically sterilized. I didn't want to prematurely go to DEFCON-5 and shut down any future possibilities, so I decided to have a Paragard IUD inserted. Much like the Ron Popeil Showtime Rotisserie, the 'set it and forget it' aspect of the IUD was very attractive to my sleep deprived self. No forgetting to take my pills, remove or insert a contraceptive ring, or deal with the visits for the shot or an insertion of an implant. 8-10 years of efficacy? Less than 1% failure rate? What's not to love? After some fighting with my insurance company to wrangle for coverage of the device, I had the IUD placed in April of 2010.
My initial excitement about the Paragard's miraculous existence was pretty quickly muted. My periods became horrendously painful two-week affairs that left me anemic and can best be illustrated using the elevator scene from "The Shining." My OB-GYN assured me it was normal, that after a few months, my body would adjust to the IUD and my cycles would shorten, the cramps would become somewhat less painful, and the bleeding would come down to a level that, while still heavy, would be far more manageable.
I stuck it out, because I wanted the Paragard to work its no-baby magic for me, and if a few months of misery was the price to pay for highly effective reversible long term birth control, I was willing to suffer.
In October, there had been no improvement. I checked with my doc, who advised that I should give the Paragard a few more months, and keep on taking my iron pills. In November, the red tsunami calmed into a far more manageable flow. I thought that I was finally home free.
In December, the flow slowed to a drizzle. I could deal with this. The drizzle, however, lasted for about three weeks. I was getting concerned, but was willing to give it a little more time, considering it was the week of Christmas, and I was busy doing Santa things and prepping for the giant sit-down meal for 15 that I was hosting.
Christmas morning went off without a hitch. I hadn't been able to keep down anything that wasn't bland and carb-y for the last month, but I have a stomach that doesn't react well with stress, so I wasn't at all concerned. I had just started a new position on November 1st, and attributed my sour stomach to stress. Christmas dinner did not agree with me, but it was par for the course.
On the Monday after Christmas, I returned to work, the drizzle still in full effect, but there was some moderate cramping ramping up as well that morning that continued to intensify throughout the day. My department was shorthanded that week, because no one ever wants to be behind a desk between Christmas and New Years. I was figuratively strapped to my chair on Monday, December 27th, 2010. This became a giant problem when I was the only person covering the phones for my office and felt a gigantic gush. I was hemorrhaging.
I looked around frantically for anyone to come back from break, and was able to flag down a coworker who was at the end of her lunch shift. As I logged out of my computer and stood up, the gush became unstoppable. By the time I had reached the bathroom, the inner thighs of my khakis were soaked in blood to my knees. If the pain weren't as bad as it was, I'd have keeled over from the sheer embarrassment of it all.
After seeing clots the size of my fist fall out of me, and trying as best I could to clean myself up to no avail, I had to trek back through the office to notify my supervisor that I had to leave. I had a hunch that my IUD may have been displaced and lodged in my uterine cavity. I called my husband to tell him I'd be driving home for a change of clothes, then we went directly to the ER. Like most Hospital Emergency Rooms in metropolitan areas, the wait was extremely long.
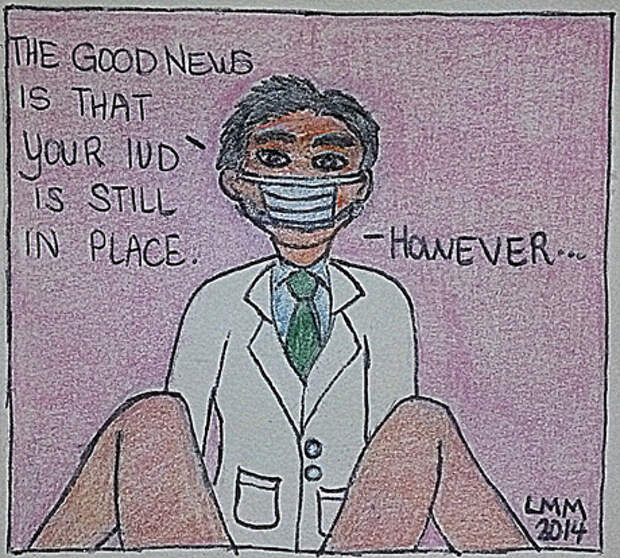
After six hours of waiting, I was taken back into a room where I was given a pelvic exam and advised that my IUD was still in place. The hospital was about to release me with advice to follow up with my OB-GYN, but when the attending doctor called my OB-GYN, he pointed out a major oversight in my treatment...There hadn't been a pregnancy test performed.
My blood was drawn and a few hours later, a nurse entered the room and advised that I was pregnant and miscarrying. Not much could be done for me, so the ER shot me up with some morphine and shoved me out of the door at 4 a.m.
Although I did not plan to have another child, and was actively seeking to avoid pregnancy, learning within a sentence that I was pregnant and losing the child was incredibly difficult. I didn't have a choice in whether I would keep the child -- it was dying, and nothing could be done to save it. It was my only miscarriage, and I could do little but sob over the baby that never had a chance. According to the blood tests, I was two months pregnant.
My OB-GYN called me at 7 the next morning after reviewing my records from the ER, advising me not to eat or drink anything, and told me to come directly to another area hospital with which he was affiliated for an emergency D&C and removal of the IUD. Walking into the Women's Center, I was surrounded by excited families anticipating the arrival of babies in the large atrium waiting area. As I was ushered to a private area by a sympathetic nurse, an excited new father burst out of the Labor and Delivery ward exclaiming "It's a boy!" to a cheering family. I didn't begrudge him his joy, but I felt like I was punched in the gut all the same. I burst into tears.
Before the D&C commenced, my OB-GYN advised that the contents of my uterus would be sent to the pathologist to ensure the pregnancy was intrauterine, but as a precautionary measure, he would inject me with methotrexate in the case of an ectopic pregnancy. Methotrexate is used in cancer patients because it attacks and dissolves abnormal cells within the body. He warned that side effects were likely, and gave me an information sheet full of misery: nausea, hair loss, loss of appetite, dizziness, and headache were pretty common. The D&C was performed without incident, and I came out of anesthesia groggy with a wildly contracting uterus. I was released home with some painkillers to await the result of the pathology report.
The next morning, my OB-GYN called to advise that there were no products of conception found within the contents of my uterus, which ensured that I had an ectopic pregnancy. He advised that the methotrexate would be the least invasive treatment, and since I had already been dosed with it, I would be best served to report to a lab every other day to ensure my hCG levels were falling consistently. For the next month, I reported for lab testing. My newly acquired job didn't afford me the time necessary to complete the testing and I was given the choice to quit or be fired when my levels didn't fall to zero quickly enough for their liking.
I quit, taking a little solace in that I had a modest savings account that provided a cushion until the ordeal was over. I was living in a melancholy cloud -- every time I didn't return with a hCG count of zero, I was reminded that I was a walking graveyard.
On the morning of January 29th, 2011, I woke determined to do something to get my mind off of my misery. My parents were to come over and keep an eye on my kids so I could go out with my husband to pick out a few lighting fixtures and grab a quiet meal without toddlers in tow. While getting ready to leave, I was struck with a searing pain in my lower abdomen that left me incapacitated and on the verge of blacking out.
I weakly called out to my husband in the next room who promptly called my OB-GYN. I was unable to dress myself, and my husband had to do it for me. Per my doctor's advice, I was driven straight to the emergency room and whisked immediately to a bed. So much for a new chandelier or a quiet lunch.
After a shot of Demerol and a sonogram, it was determined that my fallopian tube had ruptured and I had significant internal bleeding. Every move I made, no matter how small, caused the blood in my abdomen to move between my internal organs. To this day, I don't know if I'll ever experience something more painful. It feels like acid is eating away at your innards. Options were weighed and I was kept under observation and doped up on Demerol for the next 48 hours.
Because recovering from surgery would be more painful than allowing the trapped blood in my abdomen to naturally resolve itself, I chose the conservative treatment. Once the worst of the pain had subsided, and another shot of methotrexate had been administered, I was discharged from the hospital. Between the blood loss resulting from the onset of miscarriage and the internal bleeding caused by the rupture, I was severely anemic. I was weak, pallid, and severely depressed. I was lucky both times to have gotten to the hospital before I was in critical condition.
It was a draining process. I lost a baby, a job, one of my fallopian tubes, and my faith in birth control within a span of two months. I kept up my lab appointments, and the hCG levels fell more rapidly after the second dose of methotrexate. However, my hair loss and vomiting accelerated as well. I reached a blood concentration of 0 hCG about three weeks later, and I was grateful to be finished with the ordeal physically, if not yet emotionally. I was grateful that all traces of the dead fetus -- and my ill-fated IUD -- were finally gone.